Ten year history of brainstem cavernoma with six hemorrhages. 58 year old female, two years after surgery
“Before the surgery, I had blurred vision, strabismus and double vision. All these have recovered over the past six months, and now I am at home doing exercises, like climbing stairs up and down. I can feel the strength returning to my body. ”
Ms. Cooper is a retired physician. Two and a half years ago, she underwent resection of a brainstem cavernoma. At the time of her surgery, Ms. Cooper was 58 years old. She had lived with a cavernoma in her brainstem for more than ten years. She had experienced six hemorrhages, which caused symptoms such as numbness in her limbs, dizziness, tinnitus, vision loss, swallowing difficulties and others. One of the hemorrhages had even caused a cardiac arrest, a most life-threatening situation that required her to be treated in the ICU for more than 60 days.
"My pre-operative symptoms were very severe. I am so thankful to Professor Bertalanffy for doing the surgery. As a fellow physician, I got to experience Professor Bertalanffy's medical skills and his drive for technical excellence first hand. Very admirable. On the morning of the second day after surgery, my tube was removed and I woke up to see the professor. I did it! The first thing I said was:Hello, Professor Bertalanffy! Then I couldn't help but to give him a thumbs up. . . " This was two and a half years ago.
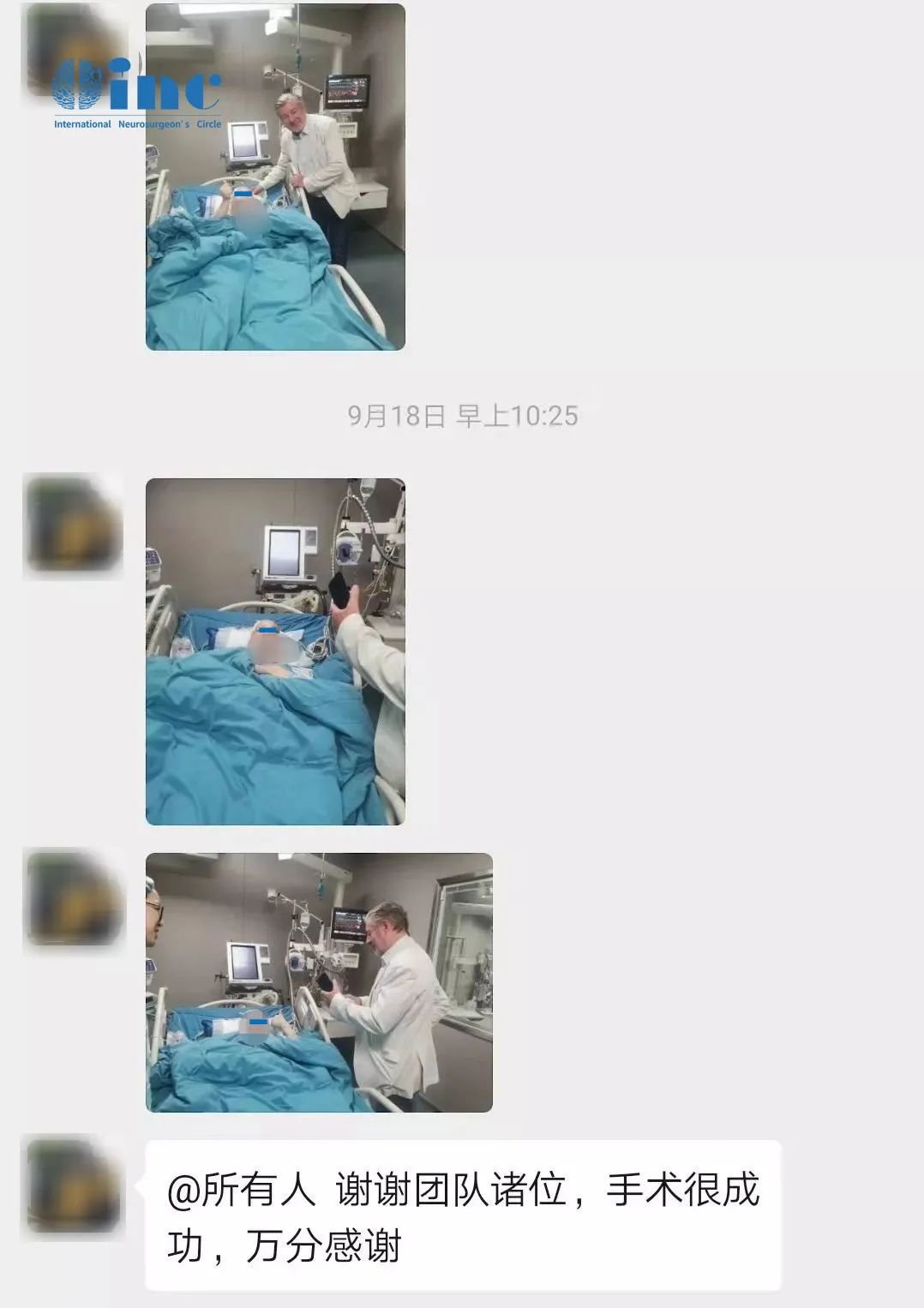
Director Cooper's family expresses their gratitude towards Professor Bertalanffy
A battle for life and death:Doctor Cooper’s painful struggle with a brainstem cavernoma
As early as 13 years ago, Doctor Cooper went to see a doctor for some discomfort in her cervical spine. The MRI scan revealed a cavernoma in her brainstem, but since she did not complain of any symptoms, she did not pay further attention to it. Then in July 2016, she first began to feel dizzy. When her left limbs became numb, she went to the local hospital again. A CT of her brain revealed that the brainstem cavernoma had hemorrhaged. Doctor Cooper subsequently visited a well-known hospital in China, where her doctor explained to her that the hemorrhage was in a very deep location and the surgical risks too high. Instead, conservative treatment was recommended to her. In October the same year, she again experienced dizziness and numbness in her limbs. She went for another CT scan at the local hospital, which confirmed another hemorrhage. Doctor Cooper was treated at the hospital and discharged after twelve days.
Then in January 2018, her original symptoms became even more severe. Now she also had difficulty swallowing. An emergency MRI scan clearly showed the hemorrhagic cavernoma in her brainstem. In February and in March, two more bleedings occurred, the last of which led to a cardiac arrest. Doctor Cooper was immediately transferred to the ICU, where emergency treatment and resuscitation were initiated. Only 66 days later did she show a level of improvement that allowed her to be discharged.
In June 2019, Doctor Cooper again experienced dizziness and numbness as well as difficulty speaking and pronouncing words. She was hospitalized for then days before she improved and could return home to recuperate. But her symptoms stayed with her, including tinnitus, numbness in the scalp, neck and left hand, stiff joints and unstable walking. On really bad days, she could only rest in bed, since standing up made her dizzy. . .
As a doctor herself, Ms. Cooper understood very well the functions of the brainstem and the dangers a cavernoma in this structure poses. Although in recent decades, neurosurgical techniques had improved considerably, and we have seen the introduction of neuro-navigation, intra-operative MRI electrophysiological monitoring and such, the brainstem is still considered a "no-go area" that is just starting to be explored surgically. Surgery is the primary choice of treatment for brainstem cavernoma, but the location still remains very challenging for doctors to operate in. There are only a handful of neurosurgeons who achieved safe total resection without causing new neurological deficits.
Doctor Cooper couldn't bear the torment and the toll the disease took on her. She was determined to find a cure. She asked around in online patient-circles, where she learned from other patients about Professor Bertalanffy. He had over 30 years of experience in brainstem surgery with more than 1, 000 successful cases, especially in the resection of brainstem cavernoma.
Professor Bertalanffy's advice:Surgery as soon as possible to eradicate the lesion
Wanting to take opportunity of Prof. Bertalanffy's coming to China to conduct surgical demonstrations, Doctor Cooper contacted the medical team of INC and applied for a slot. During her face-to-face consultation, Professor Bertalanffy said that the brainstem cavernoma should be operated as soon as possible with the aim of a complete resection, thereby minimizing chances of a recurrence. Although Doctor Cooper's brainstem cavernoma had hemorrhaged several times in the past, and she now was in a serious condition, recovery to a large degree could be achieved after a period of rehabilitation.
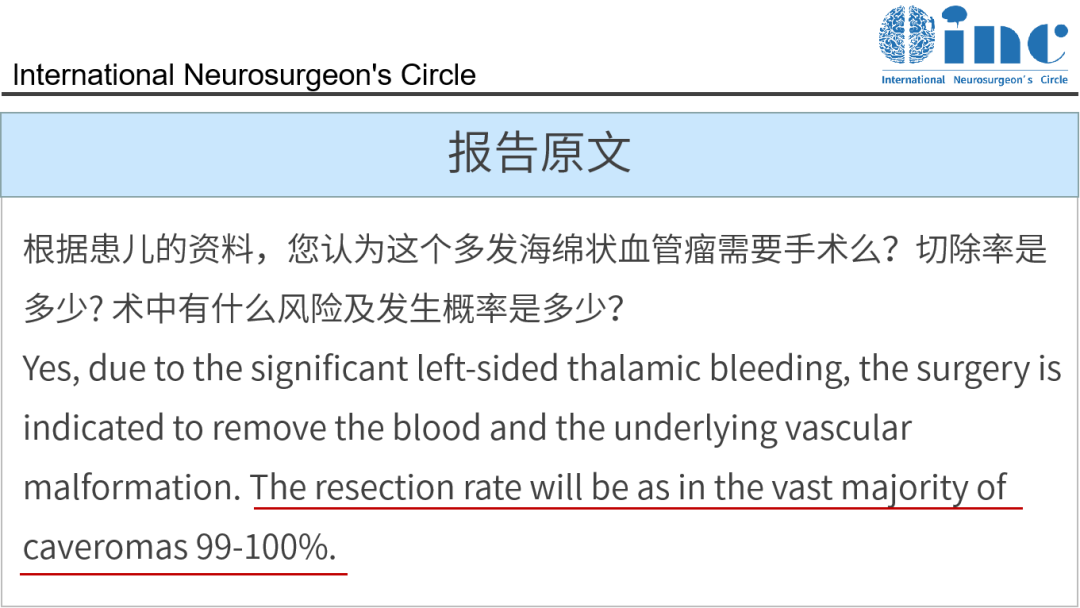
Professor Bertalanffy's response to the patient's questions
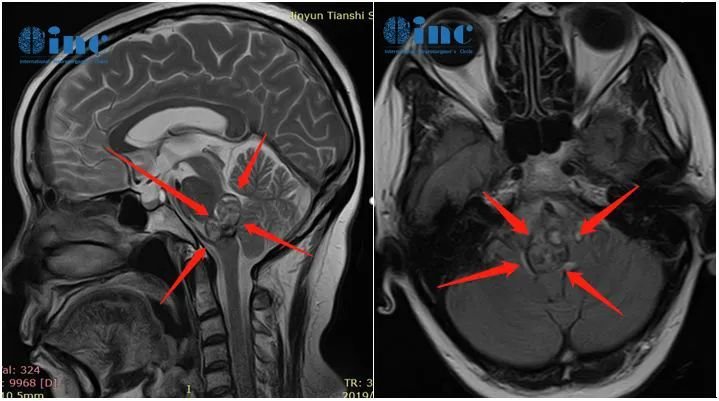
Pre-operative MRI images of Doctor Cooper's brainstem cavernoma
Very soon afterwards, INC arranged for Doctor Cooper and her family to be admitted to the Sir Run Run Shaw Hospital of Zhejiang University, where Professor Bertalanffy would perform his surgical demonstrations. Detailed preparations were undertaken, including pre-operative evaluations and discussions with Professor Bertalanffy and the local team. Finally, the surgery was safely performed.

Pre-operative case discussion at Sir Run Run Shaw Hospital with Professor Bertalanffy
The result of the operation was the complete microsurgical resection of the brainstem cavernoma. The surgery lasted for 1.5 hours and was completed without complications.
Doctor Cooper spent one day in the ICU. When she was able to breath independently again, she was extubated and returned to the normal ward on the second post-operative day. There were no new neurological deficits and no complications.
Functional status after surgery:one week after the surgery, Doctor Cooper was able to get out of bed and move around independently. Her facial numbness had disappeared, and the numbness in her scalp had improved. Her pronunciation was better than before the surgery, and she had no other post-operative complications. After ten days, her stitches were removed.
Two weeks after the surgery, Doctor Cooper was discharged.
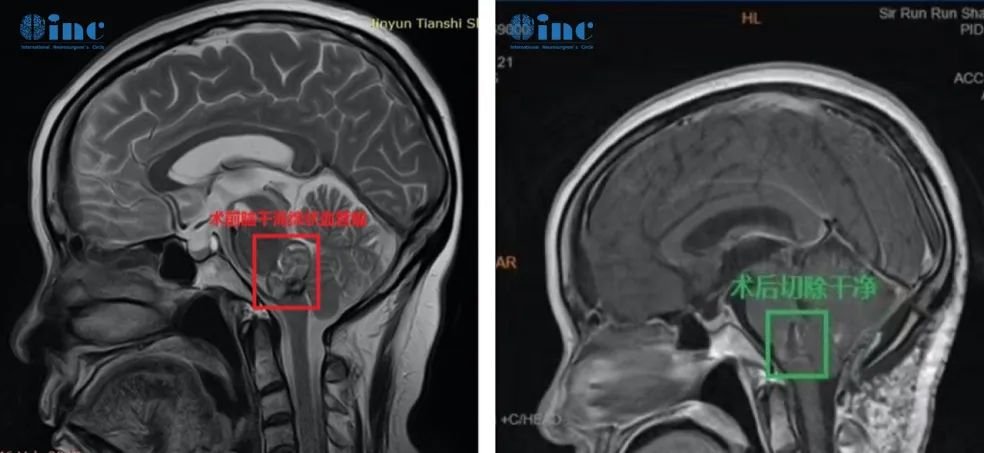
Doctor Cooper's pre-and post-operative MRI images
With the surgery successful, Doctor Cooper's brainstem cavernoma had been completely removed, eliminating any possibility of future hemorrhages and giving her the best chances at recovery and at regaining a high quality of life after surgery. Going through post-operative rehabilitation, Doctor Cooper has the best chances to recover from her pre-operative symptoms and to live a life just like any other healthy person.

INC's Professor Bertalanffy and medical team of the Sir Run Run Shaw Hospital